What is a TMD?
The temporomandibular joint (TMJ) is the name of the joint located on either side of your head, just in front of your ears. These joints connect your mandible (jawbone) to your temporal bone (skull). The TMJ, which can rotate and move forward, backward and side to side, is considered one of the most complex joints in the body. This joint, in combination with other muscles and ligaments, lets you chew, swallow, speak and yawn. When you have a problem with the muscle, bone or other tissue in the area in and around the TMJ, you may have a TMD.
Signs or symptoms of TMDs include pain and tenderness in or around the ear, the jaw joint, or the muscles of the jaw, face or temples. Other symptoms are problems opening or closing your mouth, and a clicking, popping, crunching or grinding noise when you chew, yawn or open your mouth. TMDs may be linked with neck pain and headaches. If you have any of these symptoms, tell your dentist and your doctor.
In most cases, TMDs are caused by a combination of factors like jaw injuries and joint disease, such as arthritis. It is believed that bruxism (tooth clenching or grinding) and head or neck muscle tension may make TMD symptoms worse. Stress is also a possible factor. However, it is not clear if stress causes TMDs or is a result of them.
Other things that may lead to TMDs are partial or full dentures that are not the right fit and certain habits such as fingernail biting and pen or pencil biting.
Most patients with TMDs get better by themselves without any treatment. To help ease sore jaw muscles, place a cold or warm compress to your jaw and gently massage your jaw muscles. Eat a soft diet, cut food into small pieces and avoid hard, chewy or sticky foods. Try not to open your mouth too wide, even when you yawn. And most importantly, relax your jaw muscles.
When you are relaxed, your teeth should be slightly apart and your tongue should rest on the floor of your mouth with your lips barely touching or slightly apart. There should be a slight space between your upper and lower teeth except during chewing, speaking or swallowing.
After a thorough examination and, if needed, appropriate x-rays, your dentist may suggest a plan to treat your TMD. This treatment plan may include relaxation techniques, a referral to a physiotherapist, a chiropractor or a behavioural therapist to help you ease muscle pain. Other treatment options may include medicine for pain, inflammation or tense muscles. If getting a good night’s sleep is a problem, a number of approaches to improve sleep may be used.
Your dentist may suggest wearing a nightguard, also called an occlusal splint. It is made of clear plastic and fits over the biting surfaces of the teeth of one jaw so that you bite against the splint rather than your teeth. This often helps your jaw joints and muscles to relax.
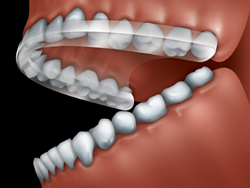
An occlusal splint is made of plastic and fits
over the biting surfaces of the teeth of one jaw.
If your pain continues, your dentist may also refer you to a dental specialist with extra training in TMDs. This could be a specialist in oral medicine or orofacial pain, an oral surgeon, an orthodontist, a periodontist or a prosthodontist. If your dentist refers you to a dental specialist, he or she will explain what that specialist does.
Surgery is rarely used to treat TMDs. However, if none of the other treatments have worked, or if it is very hard to open your jaw, you may need surgery. If you need surgery, your dentist will refer you to an oral and maxillofacial surgeon with expertise in temporomandibular joint surgery.
Get in touch
Take the first step and call us to set-up a complimentary consultation.

